Women's & Children's Hospital became one of many area hospitals Wednesday to be inundated with new patients from New Orleans, mostly neo-natal babies.
Angela Jacks, spokeswoman for Women's & Children's Hospital, said there were anywhere from 16 to 20 babies who had been transported from Tulane, their sister hospital.
Jacks could not give an exact number of how many babies they were treating, because the number keeps fluctuating.
"We're taking the most critical babies," she said, of those who could not survive the longer trips to hospitals farther away. For those who can, she said, they are assessed and then are sent elsewhere.
Many of those babies came alone; their parents and caretakers are still trapped elsewhere.
"We have some that are here; we have some that are on their way. We have some that are still stranded in New Orleans," she said.
Early Wednesday, Jacks said there were still parents who had not been tracked down. Later that day, she said their families had been contacted.
Along with those parents, there are others who are making cold calls in the hopes their loved ones have ended up there.
A woman from Cleveland, Ohio, called after she heard that her mother had been transported to a hospital within the city.
These types of calls have become common place, she said.
"We try to network with the other hospitals and try to find their family members," she said. "We can't find everybody, but we try. We do our best."
She said they've also received calls from nurses who have now become separated from their former patients.
"To be a nurse, you have to have such a good, caring heart. Just because they're letting go of the baby doesn't mean they're still not holding on to them," she said.
She said that obviously, "Right now, the hospitals' main concern is the care of the patients and getting them to a facility that can take care of them."
Jason Brown
jbrown@theadvertiser.com
The Daily Advertiser
Brandy & I would like to thank you for your thoughts, prayers and support during our time of need. Please check back often for more praise reports on Drew's status...
GOD IS FAITHFUL TO HIS WORD TO THOSE THAT PUT THEIR TOTAL TRUST IN HIM.ISAIAH 43:1-5.
Wednesday, August 31, 2005
We are fine!

We got home last night about 7:30.
Drew was flown to Women's and Childrens here in Lafayette.
Steve and I got on a cargo helicopter that was just making a supply drop at Tulane. We flew to Berwick where the helicopter base was. That was as far as they could get us. But FDF has a plant there and one of the cleaning service supervisors John drove us back home. THANK YOU John!
We are very happy to be out of all that mess and craziness. We went to see Drew last night and she is doing good. They mentioned taking her breathing tube out but I am not getting my hopes up anymore till I actually see it out.
The water was completely around the hospital at 6 feet. So there was no way we could even get out of the parking garage. Thank you to everyone who was trying to find a way to get us out of New Orleans.
Sorry this is still another short update but we are headed back out to the hospital.
Oh and Karen if you can read this please head to lafayette with all the other nurses who want to come this way. We have places for all of you to stay here. Just call Charolette's cell phone and leave a message and we will get back to you.
Charolette is staying here at our house.
For our friends and family, Charolette was Drew's nurse at Tulane and she flew in the helicopter to be with Drew for the ride.
THANK YOU everyone for all of your support and prayers.
Tuesday, August 30, 2005
Nurse, patients forced to flee
Life has changed for 28-year-old Megan Combs who, as a pediatric nurse for Tulane University Hospital, awoke at 5 a.m. Tuesday to the sight of rising water and an immediate notice that all the patients had to go.
Combs, who lives in Covington, was at Lafayette Regional Airport on Tuesday evening after being airlifted with two of her infant patients and another nurse from the hospital.
The hospital had operated through the storm by moving patients to higher floors and consolidating units, but Tuesday one of the main generators was in danger of going out. That would mean imminent death for some patients.
There were four daytime and four nighttime nurses in her unit to oversee five children. All of the children had been evacuated Tuesday.
Patients were evacuated first, then the hospital employees who could fit on the helicopters.
"Basically, it was if you could convince them to take you, you got out. If not, you stayed," she said. "There are several of our people still there. No water. No air conditioning."
Combs said the mood was controlled chaos.
"Some people were panicking," but most, she said, were very calm and knew what they had to do.
"Everyone just wanted to get out of there. No one wanted to stay," she said.
After the storm, she, along with many of her co-workers, had walked out of the front of the hospital to survey the damage. They talked about getting into their cars Monday night and going to their homes only to wake up Tuesday to find that "water was about 5 to 6 feet deep and circled the hospital."
As the helicopters lifted up to head for Alexandria, below her she could see the extent of the damage, "a lot of water, a lot of people. A lot of people on the streets are standing on overpasses that weren't flooding - just nowhere to go, wading through the water."
In her 28 years, all of which have been spent in the New Orleans area, she said she had never seen anything like it.
As for her family, she planned to meet a cousin in Baton Rouge. She was waiting for a helicopter to take her Tuesday afternoon. Her parents, grandparents and brother, however, were still in the New Orleans area. They had planned to ride out the storm at her home in Covington. She has been unable to contact them since the storm hit.
She, along with many others, has no idea what the future now holds.
"I feel like I'm in a dream. I can't even imagine what the next couple of months are going to be like."
Jason Brown
jbrown@theadvertiser.com
The Daily Advertiser
Combs, who lives in Covington, was at Lafayette Regional Airport on Tuesday evening after being airlifted with two of her infant patients and another nurse from the hospital.
The hospital had operated through the storm by moving patients to higher floors and consolidating units, but Tuesday one of the main generators was in danger of going out. That would mean imminent death for some patients.
There were four daytime and four nighttime nurses in her unit to oversee five children. All of the children had been evacuated Tuesday.
Patients were evacuated first, then the hospital employees who could fit on the helicopters.
"Basically, it was if you could convince them to take you, you got out. If not, you stayed," she said. "There are several of our people still there. No water. No air conditioning."
Combs said the mood was controlled chaos.
"Some people were panicking," but most, she said, were very calm and knew what they had to do.
"Everyone just wanted to get out of there. No one wanted to stay," she said.
After the storm, she, along with many of her co-workers, had walked out of the front of the hospital to survey the damage. They talked about getting into their cars Monday night and going to their homes only to wake up Tuesday to find that "water was about 5 to 6 feet deep and circled the hospital."
As the helicopters lifted up to head for Alexandria, below her she could see the extent of the damage, "a lot of water, a lot of people. A lot of people on the streets are standing on overpasses that weren't flooding - just nowhere to go, wading through the water."
In her 28 years, all of which have been spent in the New Orleans area, she said she had never seen anything like it.
As for her family, she planned to meet a cousin in Baton Rouge. She was waiting for a helicopter to take her Tuesday afternoon. Her parents, grandparents and brother, however, were still in the New Orleans area. They had planned to ride out the storm at her home in Covington. She has been unable to contact them since the storm hit.
She, along with many others, has no idea what the future now holds.
"I feel like I'm in a dream. I can't even imagine what the next couple of months are going to be like."
Jason Brown
jbrown@theadvertiser.com
The Daily Advertiser
Acadian transports patients from N.O.
In the next four days, as many as 2,000 patients will be transferred from New Orleans to hospitals across the state as part of Hurricane Katrina relief efforts, said Richard Zuschlag, CEO of Acadian Ambulance.
"Charity Hospital seemed to be in the worse situation because they had the oldest building and the worst damage," he said. "We had planned on using National Guard trucks to evacuate Charity, but a couple of those got bogged down. They're now using boats to get patients out of Charity out to the Causeway."
About 50 ambulances left Tuesday to begin the patient evacuation, he said.
Air ambulances transported 25 neo-natal infants from Tulane University Hospital and transported them to New Iberia, Lafayette and Alexandria, he said.
Two critical babies from New Orleans were flown to Women's & Children's' and then onto Rapides General in Alexandria with a final destination to a children's hospital in Little Rock, Ark.
Another group of medics along with Dr. Ross Judice, Acadian's medical director, were deployed to the Superdome to triage critical patients at that shelter.
"They're trying to sort out the most critical patients in the Superdome and medevac them to Baton Rouge," he said.
Fort Polk has released some of its helicopters for the mission, he said.
Meanwhile, the ambulance service has suspended its routine convalescent transfers.
"We'll take care of 911 emergencies. We're asking people to be patient with us while we're in this mode," he said.
Other hospitals in New Orleans that received less damage from Hurricane Katrina are now worried that flooding will cut off their generators, he said.
"What most people thought would be a normal hurricane was not," he said. "Hospitals were prepared for a weeklong problem, but it will be much longer."
Meanwhile, the company has had limited communications with its operations in Pascagoula and Ocean Springs, Miss.
"We're flying supplies and satellite phones out there," he said. "The biggest communication problems are Slidell and Pascagoula and Ocean Springs. It's like that area has gotten completely wiped out."
Marsha Sills
"Charity Hospital seemed to be in the worse situation because they had the oldest building and the worst damage," he said. "We had planned on using National Guard trucks to evacuate Charity, but a couple of those got bogged down. They're now using boats to get patients out of Charity out to the Causeway."
About 50 ambulances left Tuesday to begin the patient evacuation, he said.
Air ambulances transported 25 neo-natal infants from Tulane University Hospital and transported them to New Iberia, Lafayette and Alexandria, he said.
Two critical babies from New Orleans were flown to Women's & Children's' and then onto Rapides General in Alexandria with a final destination to a children's hospital in Little Rock, Ark.
Another group of medics along with Dr. Ross Judice, Acadian's medical director, were deployed to the Superdome to triage critical patients at that shelter.
"They're trying to sort out the most critical patients in the Superdome and medevac them to Baton Rouge," he said.
Fort Polk has released some of its helicopters for the mission, he said.
Meanwhile, the ambulance service has suspended its routine convalescent transfers.
"We'll take care of 911 emergencies. We're asking people to be patient with us while we're in this mode," he said.
Other hospitals in New Orleans that received less damage from Hurricane Katrina are now worried that flooding will cut off their generators, he said.
"What most people thought would be a normal hurricane was not," he said. "Hospitals were prepared for a weeklong problem, but it will be much longer."
Meanwhile, the company has had limited communications with its operations in Pascagoula and Ocean Springs, Miss.
"We're flying supplies and satellite phones out there," he said. "The biggest communication problems are Slidell and Pascagoula and Ocean Springs. It's like that area has gotten completely wiped out."
Marsha Sills
The Daily Advertiser
We are Home
By the Grace of God we are back in Lafayette with Drew.... She is doing good...
More Details to come soon ...
Thank you for all your prayers and support....
More Details to come soon ...
Thank you for all your prayers and support....
Monday, August 29, 2005
Hurricane Katrina
I spoke to Steve this morning and he said they made out ok. They don't have electricity and Canal Street has a bit of water but other than that they are fine. He asked me to update this for everyone to know they are ok, at least til he can get online. Paul
Saturday, August 27, 2005
Hurricane
Of course, just one more thing for us to worry about. We have spent a good part of today trying to get stuff in case the hurricane hits here and we lose power. The grocery store was insane! But we were able to purchase what we needed. The hospital staff said we could stay in the waiting room at the hospital during the storm.
On to more important things.
Drew is doing good! They have put off taking out her breathing tube again. They said possibly tomorrow. Her lungs are too wet, If they take out the tube today they might have to replace it. They are using the tube in the ventilator to suction fluid out of her lungs. She is now off of fentnyl which is very addictive. They had to wean her off of fentnyl by giving her methadone. Thank God she is totally off that medicine.
Friday, August 26, 2005
Closer to home
They did rounds this morning and they are lowering her pain and heart meds slowly. They decided to wait until tomorrow to remove her breathing tube just to be on the safe side. She is looking better everyday. Oh, she got some milk through her feeding tube... so that is awesome.
Thursday, August 25, 2005
Thursday update
She looks good. They dressed her up as you can see in the picture below. :)
The gave her lasiks today which gets rid of the extra fluid in her body. But it is not working like they want so she needs to pee some more to get rid of the extra fluid.
The doctor did tell us they will probably take out her breathing tube tomorrow. And the next step after that is to get her to eat. She has had a feeding this whole time so they have to get her to eat out of bottle before she goes home. Some babies forget how to eat so they have to retarin them. But I don't see Drew having a problem with it cause she still sucks on her fingers with the breathing tube in her mouth. I will update tomorrow unless something else happens tonight.
The gave her lasiks today which gets rid of the extra fluid in her body. But it is not working like they want so she needs to pee some more to get rid of the extra fluid.
The doctor did tell us they will probably take out her breathing tube tomorrow. And the next step after that is to get her to eat. She has had a feeding this whole time so they have to get her to eat out of bottle before she goes home. Some babies forget how to eat so they have to retarin them. But I don't see Drew having a problem with it cause she still sucks on her fingers with the breathing tube in her mouth. I will update tomorrow unless something else happens tonight.
Wednesday, August 24, 2005
Surgery was successful!!!!!!!!
They did not start her surgery till 10:20 today because the surgeon got stuck in traffic.
The surgery went as planned. The doctors were very happy with the outcome. The surgery did not end until about 3:30 so it has been a long day for Steve and I. She was not put in PICU until 4 and we visited with her for about 40 minutes and we left so she could get some rest without us bugging her. The surgeon did say that it is possible that the hole in her heart might close up by the time the second surgery at 7 months comes around. With God all things are possible. She looks really good, just a little puffy. Thank you for all of your prayers.
The surgery went as planned. The doctors were very happy with the outcome. The surgery did not end until about 3:30 so it has been a long day for Steve and I. She was not put in PICU until 4 and we visited with her for about 40 minutes and we left so she could get some rest without us bugging her. The surgeon did say that it is possible that the hole in her heart might close up by the time the second surgery at 7 months comes around. With God all things are possible. She looks really good, just a little puffy. Thank you for all of your prayers.
Tuesday, August 23, 2005
Tuesday Update
We just talked to the surgeon a few minutes ago.
Drew's surgery got bumped up to the first case of the day. So her surgery will be at 8 am. They have decided to go through her chest instead of through her side. Which may affect her recovery time and make it a longer journey. We will update as soon as she is out of surgery tomorrow.
The surgeon doesn't want to do anything with the hole in her heart right now because there is a possibility that it may close up on it's own, and that is what we will be praying really hard for.
Drew's surgery got bumped up to the first case of the day. So her surgery will be at 8 am. They have decided to go through her chest instead of through her side. Which may affect her recovery time and make it a longer journey. We will update as soon as she is out of surgery tomorrow.
The surgeon doesn't want to do anything with the hole in her heart right now because there is a possibility that it may close up on it's own, and that is what we will be praying really hard for.
Monday, August 22, 2005
We have a surgery date
They decided not to do the cardio cath. It was not needed.
Her surgery is set for wednesday and they said it was 2nd case. Which means she will be 2nd on the surgery list and that will be about mid morning.
This first surgery is to fix the coarctation in the aorta and put a band on a valve so her lungs don't get flooded with blood flow while we wait for the 2nd surgery in 7 months.
Just keep us in your prayers that this first surgery goes smoothly.
Her surgery is set for wednesday and they said it was 2nd case. Which means she will be 2nd on the surgery list and that will be about mid morning.
This first surgery is to fix the coarctation in the aorta and put a band on a valve so her lungs don't get flooded with blood flow while we wait for the 2nd surgery in 7 months.
Just keep us in your prayers that this first surgery goes smoothly.
Monday morning update
We got there early this morning to talk to the cardiologist who was going to do the cardio cath. He told us he did not want to do an extra procedure if it was not completely needed. So he wants to do another echo (ultrasound) on the heart to do exact measurements. It was only one doc who wanted to do the cath so she may get over ruled which is fine by me. They say that procedure is harder on little ones cause their veins are so small. So right now we are just waiting on the echo results. We will update later today.
Sunday, August 21, 2005
Sunday Update

Drew did really good today.
Tomorrow they are going to do a cardio-cath. This is a procedure where they put a line through her groin and into her heart and put dye in her to get a good picture of the heart. They have to paralize her in order to do it. They also said that it could be an all day process if they can't get a vein. So we need to pray that they can get it right away. Thank you for checking in on us.
Saturday, August 20, 2005
Name Meaning

DREW ALEXANDRA SCHAAF
Name: Drew
Origin: Old French, Greek
Meaning: sturdy, vision, strong
Name: Alexandra
Orgin: Greek
Meaning: helper & defender of mankind
Orgin: Anglo-Saxon
Meaning: Wise
Name: Schaaf
Orgin: German
Meaning: descendant of a shepherd, sheep, plane
Saturdays News
They had to put her breathing tube back in cause she was having a hard time keeping up. It was enlarging her heart a bit from it working overtime. I did get to hold her before they put it back in though. She pulled out her feeding tube last night and they had to reinsert it. And they said she is bound to pull out her breathing tube so they were going to put mittens on her hands. Once again thank you for all of the prayers.
*updated by Brandy*
*updated by Brandy*
Friday, August 19, 2005
Friday Update

She is now on 8 cc's of breastmilk. And we were so excited, WE GOT TO HOLD HER!!!!!!!!! She inow only on one medication. And that is the medication to keep her PDA valve open till surgery. She was previously one 8 other medications so this is great news. She now weighs 8 pounds 1 ounce so she is gaining weight! Visiting hours are over for the next 2 1/2 hours so we are anxiously awaiting to go back at 8:30 tonight. *updated by Brandy*
Breathing tube is out
We are about to head out the door to NO.
But I wanted to give some good news.
HER BREATHING TUBE IS OUT!!!!!!!!!!!!!!!
She is now sucking on a pacifier, which is great! She is now getting 5 cc's of milk every 3 hours. Which is very little but it's start. 30 cc's is 1 ounce so you can imagine how little 5 cc's is. Everything is looking great! Thank you God for answering all of our prayers.
But I wanted to give some good news.
HER BREATHING TUBE IS OUT!!!!!!!!!!!!!!!
She is now sucking on a pacifier, which is great! She is now getting 5 cc's of milk every 3 hours. Which is very little but it's start. 30 cc's is 1 ounce so you can imagine how little 5 cc's is. Everything is looking great! Thank you God for answering all of our prayers.
Thank You!
Dear Family and Friends,
Brandy and I want to thank you for all your prayers and support during this time of need.
As most of you know on Sunday August 15 at 11:30PM we brought Drew to the Emergency room at women’s and children’s hospital. After 1 ½ hours they were able to get a line in Drew and stabilizer her. After she was revived the ER determined she had a heart defect and needed immediate medical attention. They transported Drew to Tulane Medical Center at 11:00AM on Monday Morning.
Drew was diagnosed with a Ventricular Septal Defect (VSD) and COARCTATION OF THE AORTA.
Drew is doing great and God has made her stronger each and everyday that goes by. All of her reports have been positive. She currently is getting weaned off the ventilator and slowly coming off all medication. We praise God for the miracle he is performing in her life and ours. The Doctor will schedule surgery at the end of next week to fix her aorta. They plan to do open heart surgery once she is about 7-8 months old to fix the hole in her heart. We are praying that God will heal her heart so she doesn't have to go to surgery at all. God is so good and has given Brandy and I a peace that is unexplainable. God gave Drew to us for a reason and we are going to fulfill that reason.
Thanks again for all you prayers, love and support…
Steve, Brandy, Rylie and Drew
Brandy and I want to thank you for all your prayers and support during this time of need.
As most of you know on Sunday August 15 at 11:30PM we brought Drew to the Emergency room at women’s and children’s hospital. After 1 ½ hours they were able to get a line in Drew and stabilizer her. After she was revived the ER determined she had a heart defect and needed immediate medical attention. They transported Drew to Tulane Medical Center at 11:00AM on Monday Morning.
Drew was diagnosed with a Ventricular Septal Defect (VSD) and COARCTATION OF THE AORTA.
Drew is doing great and God has made her stronger each and everyday that goes by. All of her reports have been positive. She currently is getting weaned off the ventilator and slowly coming off all medication. We praise God for the miracle he is performing in her life and ours. The Doctor will schedule surgery at the end of next week to fix her aorta. They plan to do open heart surgery once she is about 7-8 months old to fix the hole in her heart. We are praying that God will heal her heart so she doesn't have to go to surgery at all. God is so good and has given Brandy and I a peace that is unexplainable. God gave Drew to us for a reason and we are going to fulfill that reason.
Thanks again for all you prayers, love and support…
Steve, Brandy, Rylie and Drew
Thursday, August 18, 2005
Wednesday, August 17, 2005
Ventricular Septal Defect
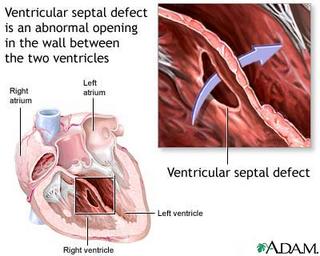
Definition:
Ventricular septal defect describes one or more holes in the muscular wall that separates the right and left ventricles of the heart -- the most common congenital (present from birth) heart defect.
Ventricular septal defect describes one or more holes in the muscular wall that separates the right and left ventricles of the heart -- the most common congenital (present from birth) heart defect.
Alternative Names:
VSD; Interventricular septal defect
Causes, incidence, and risk factors:
Before a baby is born, the right and left ventricles of its heart are not separate. As the fetus grows, a muscular wall forms to separate these lower heart chambers. If the wall does not completely form, a hole remains. This is what is known as a ventricular septal defect, or a VSD.
It is estimated that up to 1% of babies are born with this condition. In the vast majority (80-90%) of babies born with this condition, the hole is small. They will have no symptoms, and the hole will close spontaneously as the muscular wall continues to grow after birth.
If the hole is large, then too much blood will be pumped to the lungs, leading to congestive heart failure. These babies are often have symptoms related to the problem and may need medicine or surgery to close the hole.
Coarctation of the Aorta
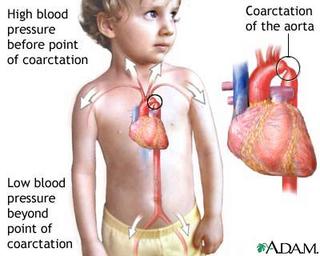
Definition:
A birth defect in which the major artery from the heart (the aorta) is narrowed somewhere along its length, most commonly just past the point where the aorta and the subclavian artery meet.
Alternative Names:
Aortic coarctation
Causes, incidence, and risk factors:
Coarctation means narrowing; aortic coarctaction is a birth defect (congenital disorder) in which a portion of the aorta is narrowed. The aorta is the source blood vessel for many arteries, which supply the body with blood and nutrients.
Aortic coarctation causes low blood pressure and low blood flow in the arteries that branch off below the narrow spot; high blood pressure occurs in the arteries that branch off closer to the heart. As a result, aortic coarctation often leads to high blood pressure in the upper body and arms (or one arm) and low blood pressure in the lower body and legs.Aortic coarctation is more common in some genetic conditions, such as Turner's syndrome, but it can also be associated with congenital abnormalities of the aortic valve, such as a bicuspid aortic valve.Aortic coarctation occurs in approximately 1 out of 10,000 people. It is usually diagnosed in children or adults under 40.
Patent Ductus Arteriosus (PDA)
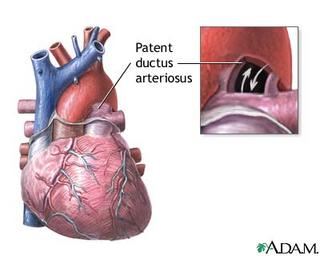
Definition:
Patent ductus arteriosus (PDA) is a condition where the ductus arteriosus, a blood vessel that allows blood to bypass the baby's lungs before birth, fails to close after birth. The word "patent" means open. Prior to birth, bloodflow in the fetus bypasses its lungs because the fetus gets oxygen through the placenta. After birth, the ductus arteriosus and foramen ovale close because blood must then go to the infant's lungs.
Alternative Names:
PDA
Causes, incidence, and risk factors:
PDA occurs in about 1 in 2,000 infants. Premature infants and those with respiratory distress syndrome are at higher risk. PDA is also associated with coarctation of the aorta, transposition of the great vessels, and ventricular septal defect.
Subscribe to:
Posts (Atom)




